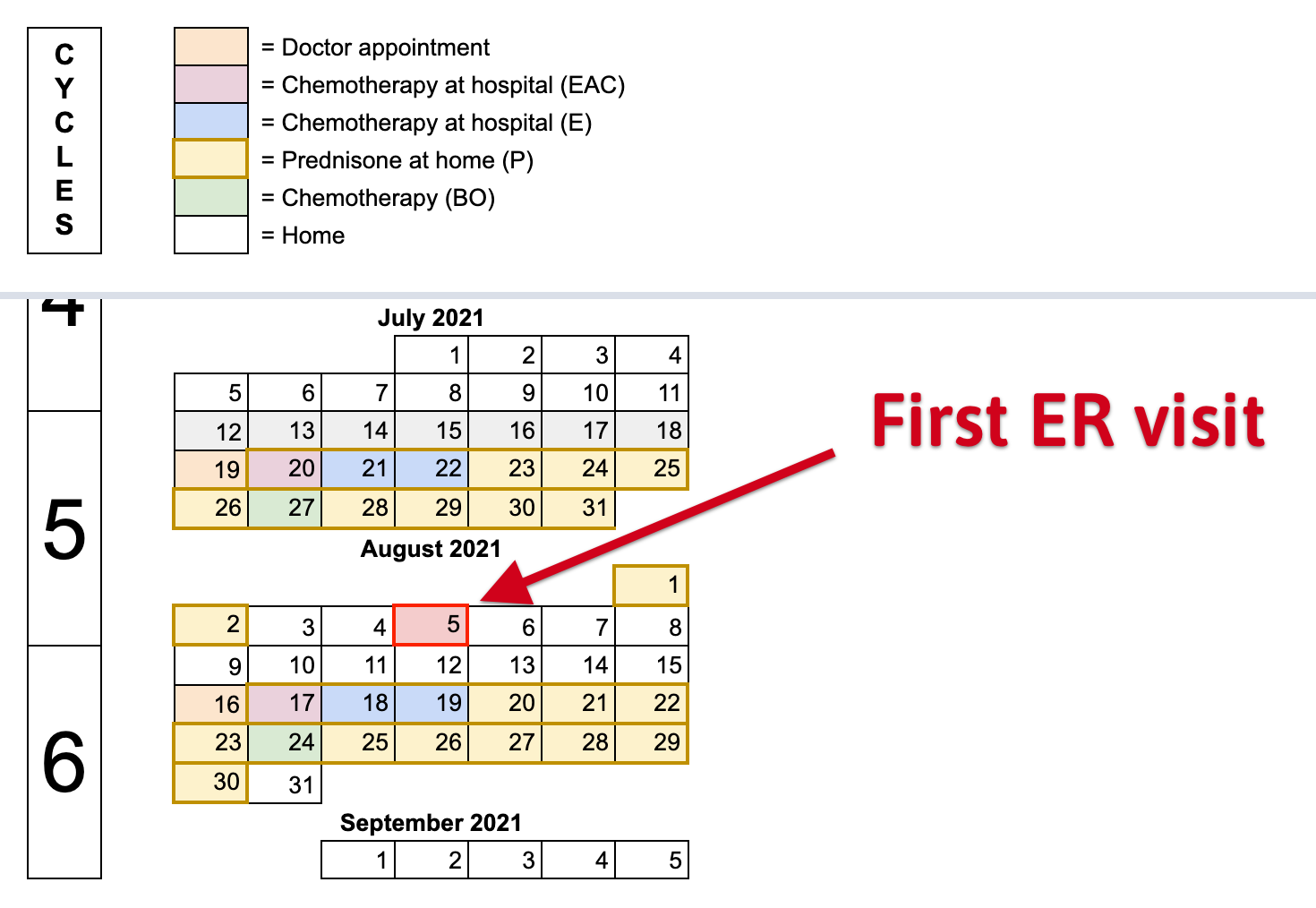
On Thursday 5th, August 2021, at 5:30pm, while resting at home I felt a bit unwell. Mimi took my temperature and I was having a fever of 38.5C (101.3F) 🤒. I took painkillers to control the fever and wait a couple of minutes. After 20 minutes, the fever went to 39.0C (102.2F). We decided to call ER oncology. The conversation over the phone was:
- Mimi: I have a patient that had chemo 8 days ago and is having a fever of 39.0C.
- ER: He should come here. However, there are a lot of patients in queue. But he should come anyway.
- Mimi: Can we visit another ER (non oncology)?
- ER: No, cancer patients are only treated here.
With no ‘many’ options, a neighbor came to brought us to the ER oncology. Before leaving, the fever went to 39.5C (103.1F). We arrived in less than 30 mins. At the ER, every cubicles were full and 2 other patients were in queue waiting for attention. A couple of minutes after arriving, a nurse came asking about the ‘patient with the fever’. She did a few routine checks on me, and took my temperature. It was 39.5C (103.1F).
One fair disadvantage that I have is that I'm usually the younger looking among others patients. The 2 other patients that were before me, was a lady in her sixties in a wheelchair and there was a man in his seventy also in a wheelchair. And I was there walking. For us, it is normal, understandable and considerate to let older patient be attended before me.
Mimi and me wasn't alone. My mother, my step-dad and my parents in law were there supporting us 🥰. I felt very grateful to have all of them with us.
Inside the ER cubicle
After 2 hours, I was admitted to the ER. By that time, the fever went down to 38.0C (100.4F) approx. The doctor and nurse ran more checks on me. Then a nurse inserted an intravenous catheter into one of my veins and then administered Paracetamol (a medication used to treat fever). Because my veins are damaged, the drip was super slow.
A couple of minutes later, a phlebotomist appeared to extract blood from my veins. However, after looking for a proper vein she couldn't find any. At that moment, the phlebotomist told the doctor that she would proceed to extract arterial blood and she repeated that to me. I didn't understand that wasn't just a message, but a warning. She punctured my body 5 times to be able to get an arterial blood sample. Most of these punctures were painful.
In the end, everything went fine at the ER. After examining my blood they prescribed a treatment for febrile neutropenia. It consisted of 3 days of: painkillers, antibiotics and Filgrastim (a medication used to treat low neutrophil count). Also, I didn't get admitted to the hospital, they allowed me to go home that same day. We left around 11:00pm.
About arterial blood
A few days later, I did some research about "arterial blood". The motivation was to understand if the pain that I experienced was to be expected. The UCSF says:
Puncture of an artery may be more uncomfortable than puncture of a vein. This is because arteries are deeper than veins. Arteries also have thicker walls and have more nerves.
When the needle is inserted, there may be some discomfort or pain. Afterward, there may be some throbbing.
That was enough to be convinced that the pain that I experienced was to be expected. Also, I think the CIPN increased the pain, because of the damage to peripheral nerves. But I'm not a doctor. I will ask my doctor about it at my next appointment.